Edge Collective
Ventilation and reducing the risk of COVID transmission
DIY ventilation assessment and improvement in order to reduce the risk of airborne disease transmission.Indoor Ventilation Assessment and Improvement
(Updated: 2021-07-23 12:37:54 )
Overview
- COVID-19 is now known to be 'airborne', which has implications for how it is transmitted, and how to mitigate the risk of contracting it.
- The intuition we should now have for our viral exposure is more akin to e.g. inhaling cigarette smoke than to droplets from e.g. a spray bottle
- A relatively air-tight room can therefore pose a significant transmission risk, even if the infected person is located on the other side of the room.
- Most masks are more effective at preventing the wearer from sending particles into the room than at preventing viral particles from being inhaled by the wearer.
- It currently (June 2021) appears likely that those fully vaccinated with the Pfizer and Moderna vaccine who experience breakthrough infections are able to transmit the disease to others.
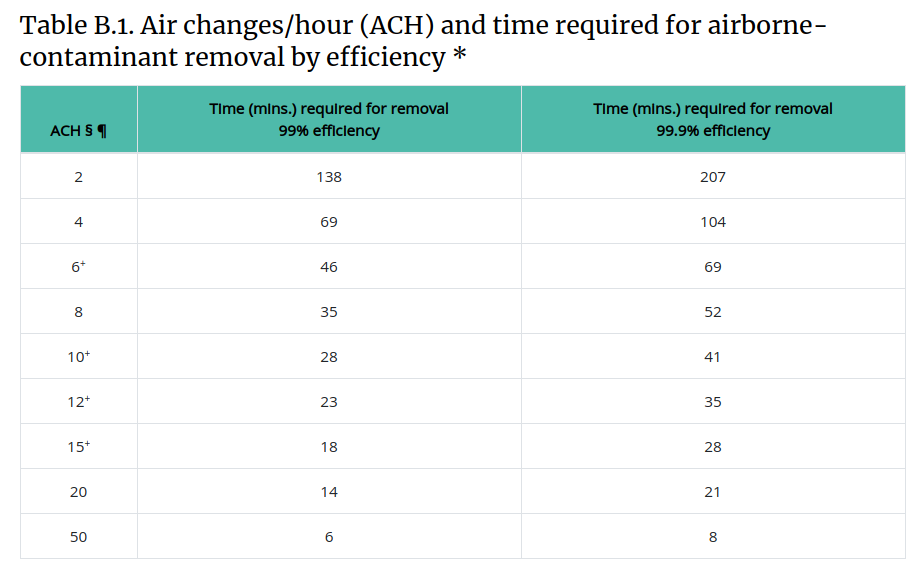
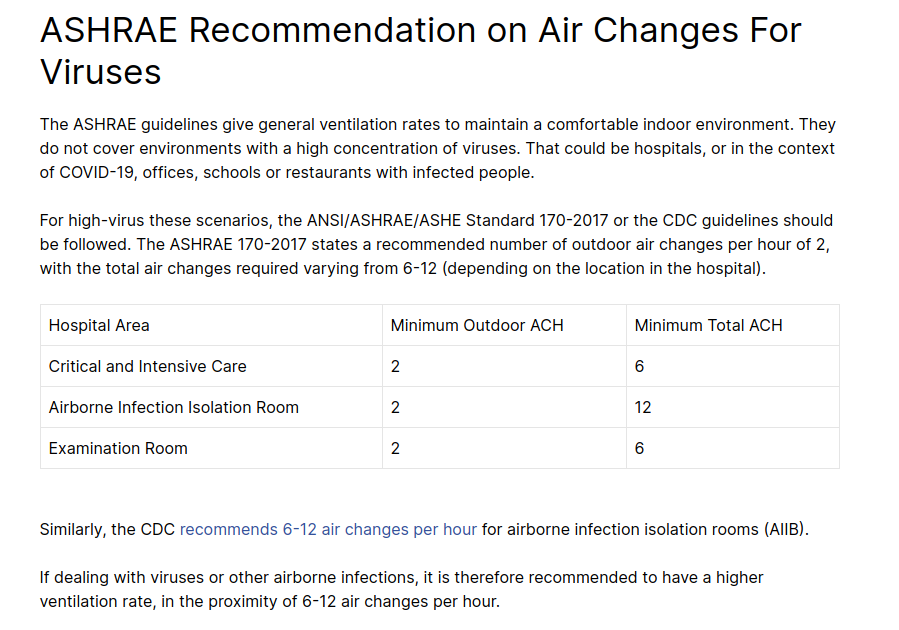
- Hospitals aim for a minimum of 6-12 ACH, with studies showing improvements up to 20 ACH (but not really beyond that).
DIY Ventilation / Corsi Boxes
SmartAir Instructions
https://smartairfilters.com/en/blog/diy-purifier-effectivness/
Nice graphs, incuding graph of particulate sized captured by filter: https://smartairfilters.com/wordpress/wp-content/uploads/2020/12/MERV-Filters-Capture-Nanoparticles.jpg
Energy Vanguard
https://www.energyvanguard.com/blog/how-make-high-merv-diy-portable-air-cleaner/
John Semmelhack
With tests of performance characteristics.
https://twitter.com/JohnSemmelhack/status/1313859125206548481?s=20
Video guide
https://www.youtube.com/watch?v=Y7eL2OAnqc8
Testing re: particle size capture
Pirie associates instructions
Nice article with good references https://www.pirieassociates.com/blog/diy-box-fan-filter
Student-built
https://twitter.com/DrEricDing/status/1363868394391539712?s=20
WIRED Article
"Could a Janky, Jury-Rigged Air Purifier Help Fight Covid-19?": https://www.wired.com/story/could-a-janky-jury-rigged-air-purifier-help-fight-covid-19/
Tex-Air Filters
"A Variation on the “Box Fan with MERV 13 Filter” Air Cleaner": https://www.texairfilters.com/a-variation-on-the-box-fan-with-merv-13-filter-air-cleaner/
"How to Improve the Efficiency of the “Box Fan and MERV 13 Filter” Air Cleaner": https://www.texairfilters.com/how-to-improve-the-efficiency-of-the-box-fan-and-merv-13-filter-air-cleaner/
Improving effectiveness of corsi air box using a shroud: https://www.texairfilters.com/how-to-improve-the-efficiency-of-the-box-fan-and-merv-13-filter-air-cleaner/
Corsi air box with five filters: https://www.texairfilters.com/a-variation-on-the-box-fan-with-merv-13-filter-air-cleaner/
Using ppm with filters: https://www.texairfilters.com/its-all-about-the-air-flow-through-the-filter/ -- makes ppm assessment
Good pics of box fan here https://www.texairfilters.com/a-variation-on-the-box-fan-with-merv-13-filter-air-cleaner/
Public Health Guidelines on Ventilation
Rhode Island Covid air filtration
https://covid.ri.gov/covid-19-prevention/indoor-air-circulation
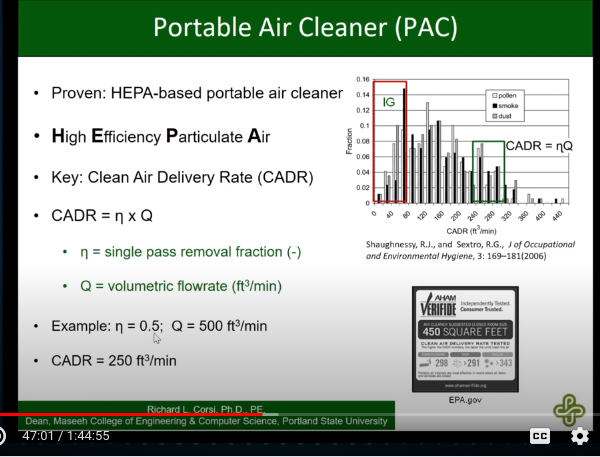
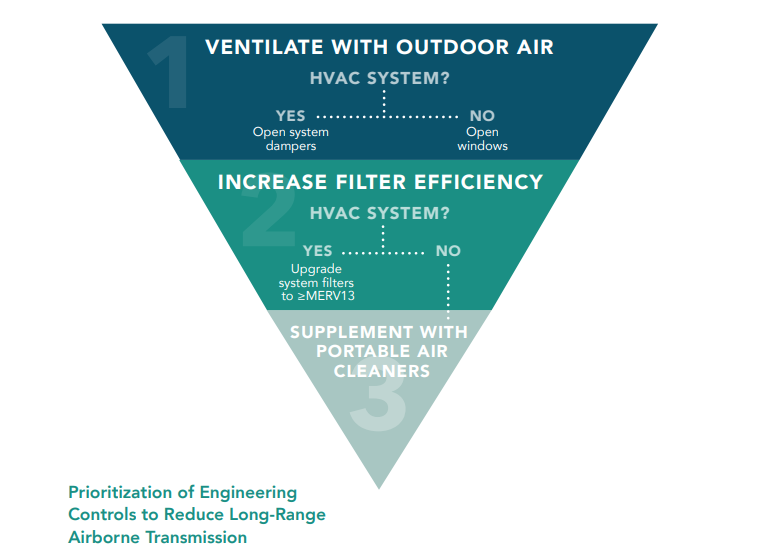
Ventilation with recirculated air will not reduce the risk of COVID-19 unless that recirculated air goes through a filter that is made to get rid of tiny particles. A filter’s Minimum Efficiency Reporting Values (MERV) rating describes how well it removes different sized particles in the air. A MERV rating of 13 or higher (MERV 13+) means that the filter gets rid of at least 90% of the particles the size of virus-containing aerosols. High Efficiency Particulate Air (HEPA) filters are designed to exceed the highest MERV rating. A HEPA filter gets rid of at least 99.97% of particles that are even smaller than aerosols.
Havard School of Public Health Ventilation Assessment guide
They describe the CO2 method as well
They recommend at 6+ ACH.
Recommended ACH in hospitals / health care facilities
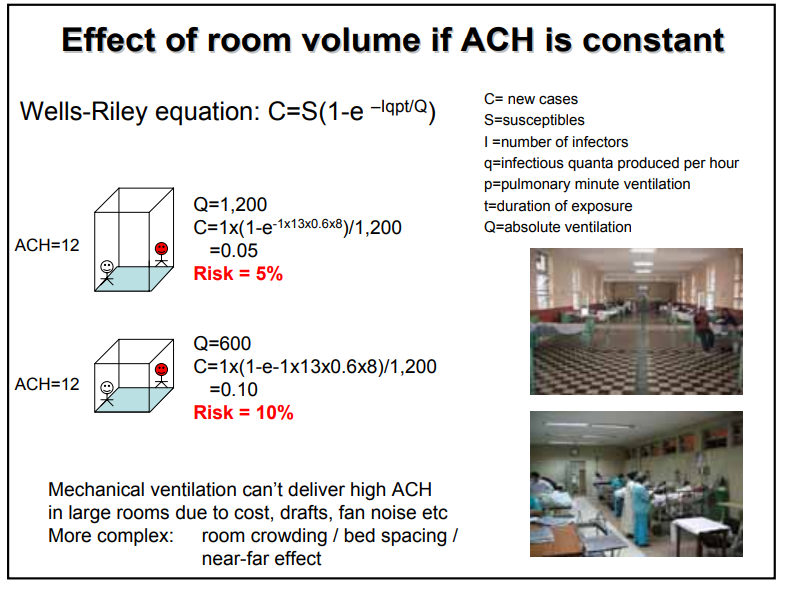
Due to variations in state building codes, 15 or 20 air changes per hour (ACH) may be the minimum required. However, in practice, most hospitals operate at 20 to 25 ACH with some using up to 40 ACH. These rates are all up from 12 ACH, which was the requirement for many years. By comparison, the requirement for patient rooms is 6 ACH.
Overall, the team found that 20 ACH had statistically significantly fewer particles and CFUs than 15 ACH. However, for the most part, 25 ACH did not provide significantly cleaner air than 20 ACH. For particles, one OR showed no statistical difference among 15, 20 or 25 ACH at all particle sizes, while another OR showed significantly cleaner air at 20 than at either 15 or 25. There was an isolated case with the more dispersed diffusers in which 25 ACH produced more particles than lower ventilation rates. The team could not confirm the cause of this phenomenon, but have seen other research indicating that higher ventilation rates can cause or “stir up” more airborne particles.
https://www.cdc.gov/infectioncontrol/guidelines/environmental/appendix/air.html
"Indoor Air Changes and Potential Implications for SARS-CoV-2 Transmission": https://jamanetwork.com/journals/jama/fullarticle/2779062
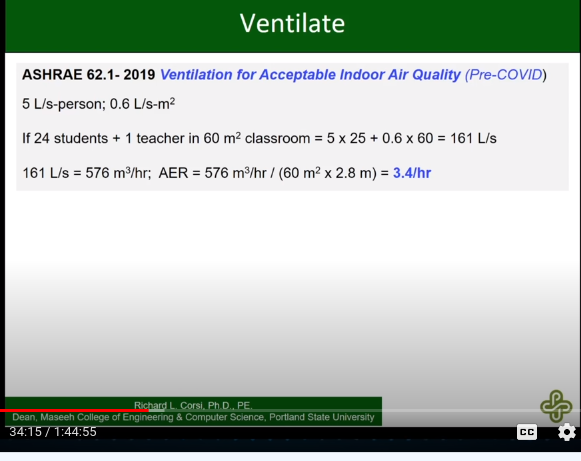
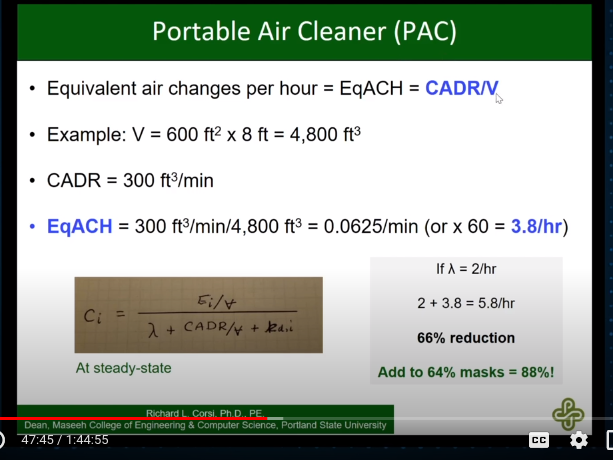
To reduce far-field airborne transmission of SARS-CoV-2 in small-volume indoor spaces (eg, classrooms, retail shops, homes if guests are visiting), the suggestions include targeting 4 to 6 air changes per hour, through any combination of the following: outdoor air ventilation; recirculated air that passes through a filter with at least a minimum efficiency rating value 13 (MERV 13) rating; or passage of air through portable air cleaners with HEPA (high-efficiency particulate air) filters.
Despite the dose-response for SARS-CoV-2 being unknown, and continued scientific debate about the dominant mode of transmission, evidence support these suggestions. First, SARS-CoV-2 is primarily transmitted from the exhaled respiratory aerosols of infected individuals. Larger droplets (>100 μm) can settle out of the air due to gravitational forces within 6 feet, but people emit 100 times more smaller aerosols (<5 μm) during talking, breathing, and coughing. Smaller aerosols can stay aloft for 30 minutes to hours and travel well beyond 6 feet.1 Second, high-profile and well-described SARS-CoV-2 outbreaks across multiple space types (eg, restaurants, gyms, choir practice, schools, buses) share the common features of time indoors and low levels of ventilation, even when people remained physically distanced
- nice review -- includes discussion of CADR and ACH
"COVID-19 Outbreak and Hospital Air Quality: A Systematic Review of Evidence on Air Filtration and Recirculation": https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7489049/
Useful graph of MERV ratings: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7489049/figure/fig2/
The combination of HEPA filtration and air recirculation has been shown to be extremely effective in many space functions such as ORs, AIIRs, and PEs. These systems clean air by simultaneously removing (i.e., filtering) and diluting (through recirculation) contaminants from the space.
"Heating, ventilation and air conditioning (HVAC) in intensive care unit": https://ccforum.biomedcentral.com/articles/10.1186/s13054-020-02907-5
- suggests that operating rooms have a minimum of 20 ACH
"ASHRAE Healthcare FAQ": https://www.ashrae.org/technical-resources/healthcare-faq
Currently, ASHRAE Standard 170 requires 6 total ACH for Gastrointestinal Endoscopy procedure rooms. There is no pressure requirement. Airflow may not be recirculated within the room.
If the procedure is an aerosol generating procedure, regardless of whether it is on a COVID-19 positive patient or not, it is recommended to perform the procedure in an airborne infection isolation room or a bronchoscopy room. ASHRAE Standard 170 requires 12 total ACH for Bronchoscopy rooms. The room must be negative, 100% exhaust, and no recirculation within the room.
CDC: "Airborne Contaminant Removal" as a function of ACH
https://www.cdc.gov/infectioncontrol/guidelines/environmental/appendix/air.html
"Role of air changes per hour (ACH) in possible transmission of airborne infections": https://www.orf.od.nih.gov/TechnicalResources/Bioenvironmental/Documents/RoleofACHinTransmissionofAirborneInfections508.pdf
ASHRAE 170 2008 and the CDC guidelines 2005 recommend ventilation rates of minimum 12 ACH for hospital insulation rooms. Although increasing ventilation airflow rate does dilute concentrations better when the contaminant source is constant, it does not increase ventilation effectiveness.
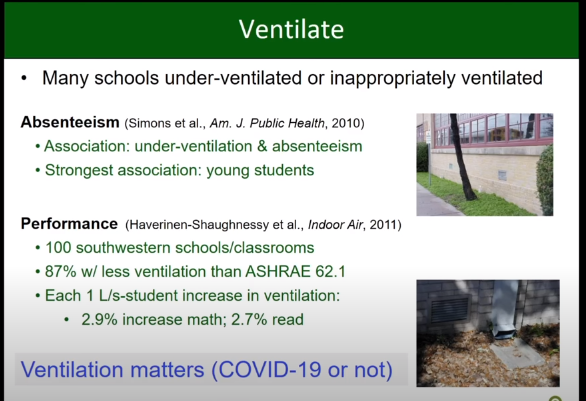
"Recommended ventilation rates for homes, offices, schools, more": https://smartairfilters.com/en/blog/ashrae-per-hour-office-residential-school-virus/
Consumer analysis critique of using ACH as a metric for indoor ventilation when assessing air purification:
https://www.consumeranalysis.com/guides/air-purifiers/ach/
WHO natural ventilation guide: https://www.who.int/water_sanitation_health/publications/natural_ventilation.pdf
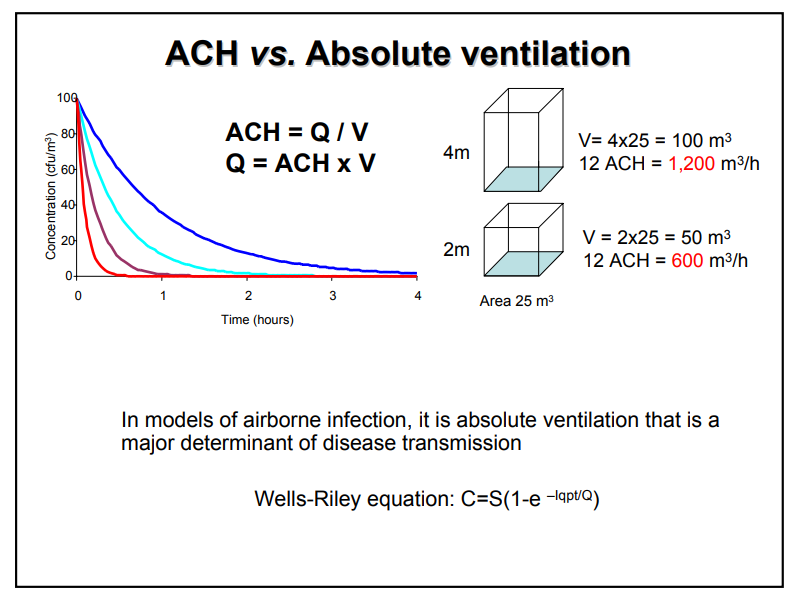
Interesting: they speak of "liters per second per patient" -- which seems like a better statistics than ACH.
Note too: we see in more than one reference that "ACH" should depend on occupancy of a room.
CO2 Monitoring to Assess Indoor Ventilation
Why is CO2 Monitoring Useful?
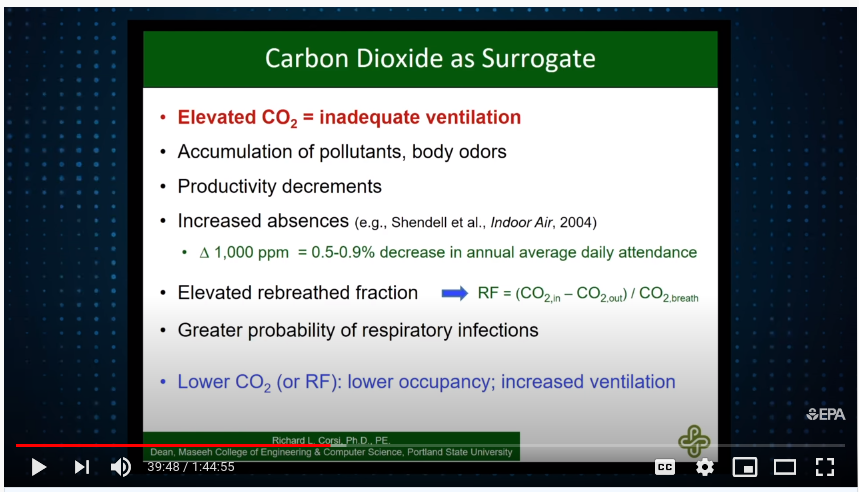
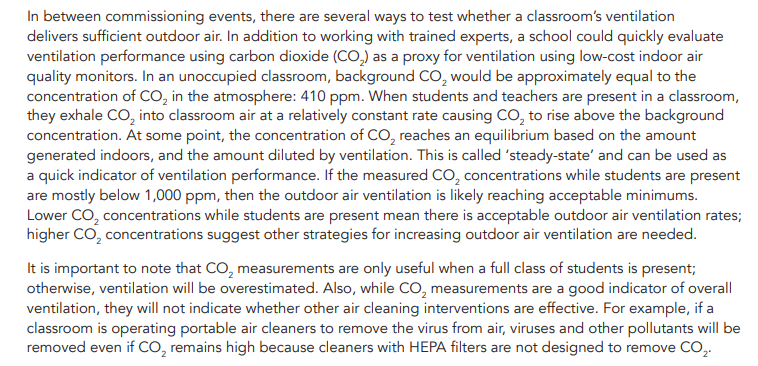
CO2 monitoring has long been used for determining the effectiveness of indoor residential ventilation. Changes in indoor CO2 concentration can indicate whether air inside a room has 'refreshed' since its most recent occupants left, or whether there is sufficient space and/or ventilation inside a building that people are unlikely to spread airborne illness.
CO2 can also be used as a 'tracer gas' to determine the rate of ventilation in a given space, usually assessed in "air changes per hour" (ACH).
Jimenez et al
"Exhaled CO2 as COVID-19 infection risk proxy for different indoor environments and activities"
https://www.medrxiv.org/content/10.1101/2020.09.09.20191676v1.full.pdf
Washpost on CO2 monitoring trend
https://www.washingtonpost.com/health/2021/02/10/carbon-dioxide-device-coronavirus/
Dustin Poppendieck
Main twitter thread on ACH: https://twitter.com/Poppendieck/status/1366055136859070468?s=20
-
need to account for other sources of indoor CO2
-
snapshot CO2 measurements don't help you predict impact of additional occupants on concentration, and thus make it hard to know how safe a space is
-
Havard School of Public Health suggests at least 5 or 6 air changes per hour
-
Recommends getting CO2 level up to 1000 ppm to 1500 ppm
-
Can get sense of variation in fit by fitting slightly different regions. Don't report more than one decimal place.
-
ACH can change by factor of 5-10 depending on indoor-outdoor temp difference, windspeed (at least at low ach) https://twitter.com/Poppendieck/status/1366055181578694657/photo/1
-
Having neighboring connected rooms empty tends to overestimate the ACH; having neighboring connected rooms occupied will tend to underestimate the ACH.
-
HVAC can mix rooms with other rooms, adding complication.
-
CO2 monitors need to be calibrated frequently to avoid drift in absolute measurements; but relative measurements tend to be solid.
-
need to acknowledge additional sources of CO2.
Menzies et al 1995
Uses precisely the method. Compares windows / doors condition.
Findings:
- use a fan during release of co2 to homogenize measurements throughout room; don't need to do afterward.
Good mixing of the tracer gas is important to ensure that the decline in concentration reflects dilution from air exchange and not simply continued mixing within the room. Evidence of good mixing was provided by minimal variation between different sites in the same room in the preliminary study, linear decay of the log-transformed concentration of CO 2 (log data not shown), and by reproducibility of repeated measures of air-change rate. All of these conditions were met when a large fan was operated dur- ing the release, meaning that this aspect of the protocol was es- sential to achieve accurate reproducible estimates of air-change rates. (p 1999)
-
They reference the impact of having a practitioner in the room while monitoring decay. Need to review this. Good reason to have data collection remote.
-
One of their fitting methods stops within 2 SD of baseline.
Huang et al
They do a CO2 experiment with baking soda and etc in dental offices.
One big impact is that they show that this method compares favorably with calculating ACH using CFM assessment at vents.
Stir mixture for 2 minutes, then remove from room.
Small oscillating fan was used to keep CO2 well-mixed in room.
They use a simpler method for determing the decay -- 'the time needed to remove 63% of excess CO2'. Method described bottom p 11 top of p 12.
They indicate that the CO2 method is a better measurement than CFM ventilation rate (p 12).
Roulet et al
Nice presentaiton of the log fit method
Escombe / tropical medicine presentation
https://www.ghdonline.org/uploads/Measuring_Air_Changes.pdf
"Wells-Riley equation"
They use a graph indicating the difference between windows opened and windows closed.
They use fire extinguishers to generate enough CO2.
They also use fans to guarantee mixing.
Can also use jackets.
They stop within 200 ppm of baseline.
p 8 and 9 are key: it's not just relative ACH, it's absolute ventilation that is the key determinent of risk.
Using Wells-Riley Equation with COVID-19
"Assessing and controlling infection risk with Wells-Riley model and spatial flow impact factor (SFIF)": https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7834120/
DIY CO2 Monitoring
Ongoing notes on development of a free-and-open-source CO2 monitor are posted here.
Feigl-Ding
COVID-19 and Schools
UC Berkeley Curated List
"UC Berkeley: COVID-19: RESOURCES FOR REOPENING HEALTHY SCHOOL FACILITIES": https://citiesandschools.berkeley.edu/covid-school-facilities
Classroom Ventilation and Transmission Risk
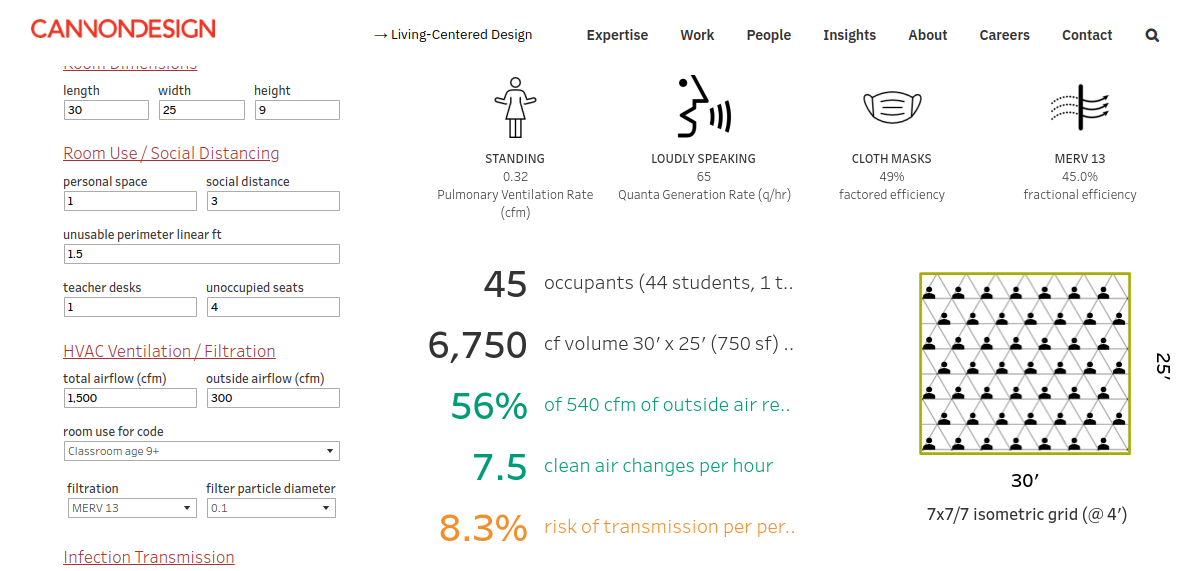
"Live" model from Cannon Design: https://www.cannondesign.com/covid-transmission-risk/
EPA Webinar -- Classroom Layered Risk
https://www.youtube.com/watch?v=SPfHpHRJN9g
Corsi's contribution: https://youtu.be/SPfHpHRJN9g?t=687
Reduce speaking -- order of magnitude more emissions than if just breathing:
https://youtu.be/SPfHpHRJN9g?t=1498: 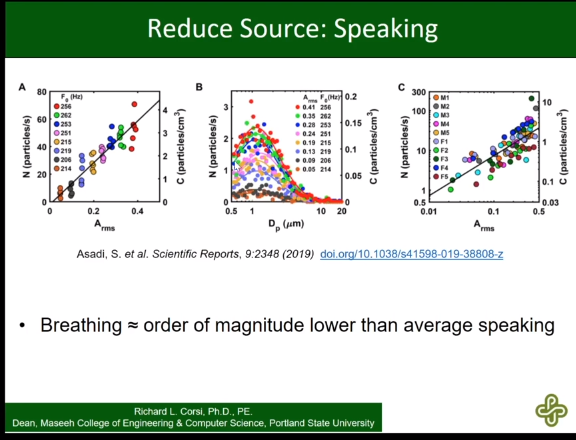
https://youtu.be/SPfHpHRJN9g?t=2055:
Calculating rebreathe fraction:
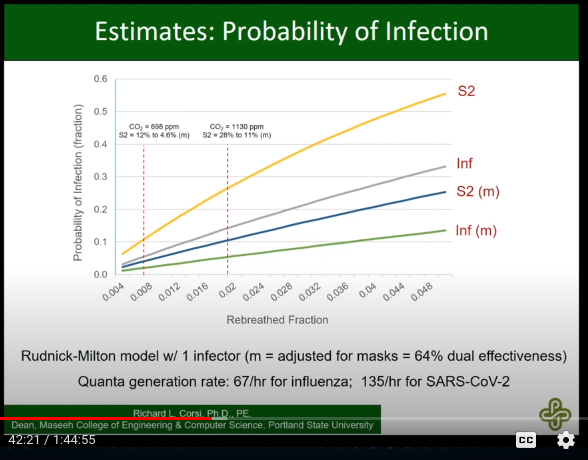
CADR:
equivalent ACH (supports our assessment):
---> the key point --->
https://youtu.be/SPfHpHRJN9g?t=2884
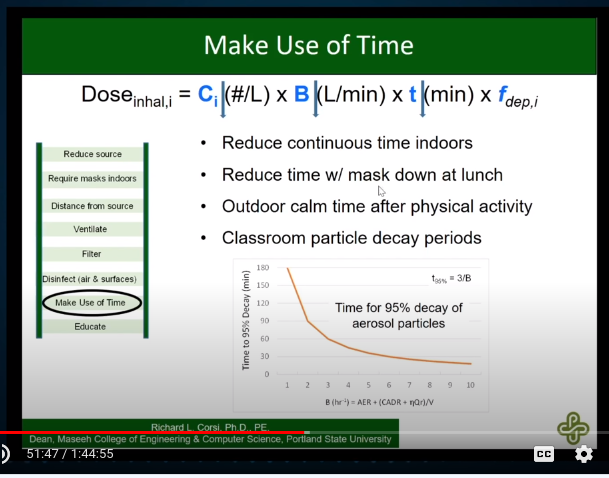
reducing time indoors:
ASHRAE position statement on infectious aerosols: https://www.ashrae.org/file%20library/about/position%20documents/pd_infectiousaerosols_2020.pdf
WHO on ACH
https://youtu.be/XJC1f7F4qtc?t=161

ACH definitions / fundamentals
https://en.wikipedia.org/wiki/Air_changes_per_hour
Individual Domain Experts / Commentators
Air-Quality-COVID-Science Twitter List
https://twitter.com/i/lists/1337064747762642947
Delta variant / viral load
Evidence for COVID being airborne
Study: 85% of viral load transmitted by COVID-19 patients is 5um or smaller
https://twitter.com/AliNouriPhD/status/1424035540022829062?s=20
Lancet article in support of aerosol spread
https://www.thelancet.com/journals/lancet/article/PIIS0140-6736(21)00869-2/fulltext
If an infectious virus spreads predominantly through large respiratory droplets that fall quickly, the key control measures are reducing direct contact, cleaning surfaces, physical barriers, physical distancing, use of masks within droplet distance, respiratory hygiene, and wearing high-grade protection only for so-called aerosol-generating health-care procedures. Such policies need not distinguish between indoors and outdoors, since a gravity-driven mechanism for transmission would be similar for both settings. But if an infectious virus is mainly airborne, an individual could potentially be infected when they inhale aerosols produced when an infected person exhales, speaks, shouts, sings, sneezes, or coughs. Reducing airborne transmission of virus requires measures to avoid inhalation of infectious aerosols, including ventilation, air filtration, reducing crowding and time spent indoors, use of masks whenever indoors, attention to mask quality and fit, and higher-grade protection for health-care staff and front-line workers.2 Airborne transmission of respiratory viruses is difficult to demonstrate directly.3 Mixed findings from studies that seek to detect viable pathogen in air are therefore insufficient grounds for concluding that a pathogen is not airborne if the totality of scientific evidence indicates otherwise. Decades of painstaking research, which did not include capturing live pathogens in the air, showed that diseases once considered to be spread by droplets are airborne.4 Ten streams of evidence collectively support the hypothesis that SARS-CoV-2 is transmitted primarily by the airborne route.5
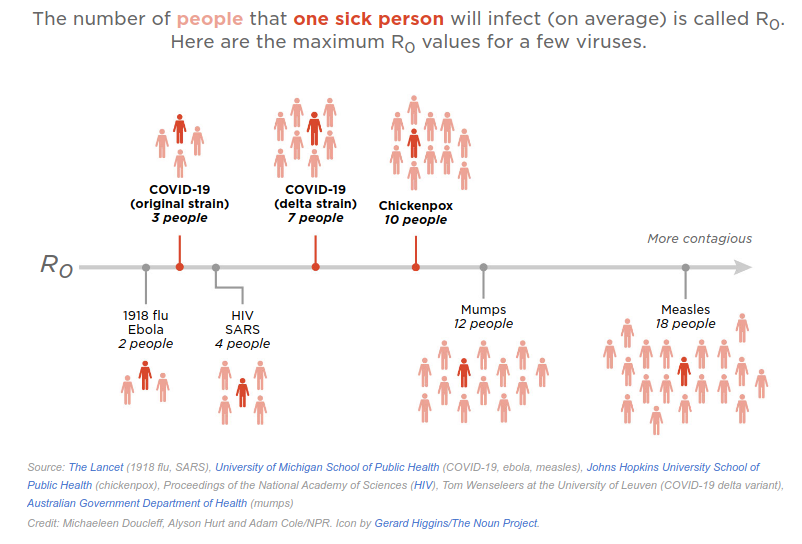
Contagiousness of Delta Variant
Coleman et al. 06 Aug 2021
"Viral Load of SARS-CoV-2 in Respiratory Aerosols Emitted by COVID-19 Patients while Breathing, Talking, and Singing": https://academic.oup.com/cid/advance-article/doi/10.1093/cid/ciab691/6343417
Associated summary Twitter thread: https://twitter.com/drkristenkc/status/1423801687513333762?s=20
Alex Huffman / viral aerosols transmission outdoors / concerts
https://twitter.com/HuffmanLabDU/status/1423864836891365377?s=20
Corsi on COVID-19 being airborne
"From the beginning of the pandemic, in the United States, there were six to eight of us trying to get the message out that this looks airborne to us," said Dr. Richard Corsi.
"It's not just close contact and it's not just contaminated surfaces," Corsi explained. "It's also what I call 'far field' contact, which is if you're not standing 3 or 6 feet from a person but you happen to be in the same crowded restaurant or the same crowded bar or a classroom and you're not near the infector ... you can inhale aerosols, droplet nuclei that contain infectious viruses in them."
That's because when someone who is infected coughs or even simply talks, tiny respiratory droplets are emitted into the air. If the space is not well-ventilated those particles can build.
"The levels just keep accumulating and accumulating and accumulating to higher and higher levels in that indoor space," Corsi said.
The scientists are calling for WHO to revise its recommendations and warn that these aerosols can potentially infect people so they can take the necessary steps to protect themselves and others.
"We need to ventilate more, we need to use better filtration systems, we need to use ultraviolet radiation in some cases, we should be using portable air purifiers in some cases," Corsi said.
Corsi also says we should all be wearing face coverings, and establishments should be limiting the number of people allowed inside at any given time.
General references on air cleaning / purifiers
Sciencenews on air cleaning
https://www.sciencenews.org/article/coronavirus-covid-air-spread-indoor-clean-ventilation-filtration
Curtius et al -- testing mobile air purifiers
https://www.tandfonline.com/doi/full/10.1080/02786826.2021.1877257
Impact of HEPA filters
https://twitter.com/DrEricDing/status/1363731992068644864?s=20
Relative effectiveness of purifiers
great graph re: impact of purifiers https://twitter.com/DrEricDing/status/1363638397684842496/photo/1
General notes on ventilation
Dr. Jiminez thread reviewing Science publication on COVID as airborne disease
https://twitter.com/jljcolorado/status/1430967286244970502?s=20
Jiminez Science review 27 Aug 20201
http://science.sciencemag.org/content/373/6558/eabd9149/tab-article-info
Risk Reduction Strategies for Reopening Schools (Harvard TH Chan)
Smoke ventilation visualization
https://twitter.com/DrEricDing/status/1363767569996541952?s=20
Synergist 'Ventilation checklist'
Very nice background:
https://synergist.aiha.org/202012-a-ventilation-checklist
"How to ventilation for COVID 19"
https://herf.medium.com/how-to-ventilate-for-covid-19-c8ce1bd13300
Link to Zeynep's article; readable background. Reinforces 6-12 ACH figure.
Increasing Ventilation By Changing Occupancy Patterns
"Occupancy-aided ventilation for both airborne infection risk control and work productivity": https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7718782/
Delta Variant
"4 Reasons Why I'm Wearing a Mask Again": https://twitter.com/Boghuma/status/1418276227664711681?s=20
"Why Vaccinated People Are Getting Breakthrough Infections" https://twitter.com/apoorva_nyc/status/1418250362193055747?s=20
In the vast majority of causes breakthrough infections are mild to asymptomatic and not a problem for the vaccinated person. But some evidence suggests they may still pass the virus on to others.
The Delta variant has turned suburban streets into a @NASCAR track. Seatbelts might be enough to keep you safe when you're driving in your suburban neighborhood, but if you're a NASCAR driver, you also want a helmet, airbags, and more.
https://twitter.com/apoorva_nyc/status/1418251783315542021?s=20
The CDC says it is not revising its mask guidance, and points out that local leaders can make their own decisions based on community rates. But every expert I spoke to for this story (about a dozen) said they have continued to wear masks and socialize mostly outdoors.
Joaquín Beltrán
"Part 3: Delta Variant Hot Surge Summer in the U.S.": https://joaquinlife.medium.com/part-3-delta-variant-hot-surge-summer-in-the-u-s-4fc7538bdc25?source=social.tw
US Dept of Ed COVID-19 Guidelines
"Improving ventilation" https://www.ed.gov/coronavirus/improving-ventilation
Misc
TODOS:
Need to figure out impact of having different sized holes on co2 apparatus.
-
Presentation / tropical medicine / effect of room size?
-
Recommended ACH for COVID / H-SPH?
-
Find space where can measure air flow at vents to test ACH determination method?
-
We saw that propane and indoor heating were complications at artisan'
-
Air flow direction on MERV 13 filters?
-
Response time of CO2 sensors?